Abstract
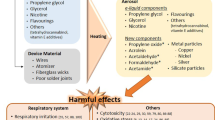
Cardiovascular disease is the major cause of death in smokers. Although new tobacco products such as e-cigarettes do not generate many of the harmful or potentially harmful constituents (HPHCs), present in combustible tobacco products the cardiovascular effects of these devices are unknown and their efficacy in promoting and sustaining cessation remains unclear. Currently, these devices are being marketed as cleaner and safer alternative to smoking that could help smokers quit smoking. Nevertheless, e-cigarette aerosols contain appreciable levels of carbonyls, which within the concentration range reported in e-cigarettes, exert significant cardiovascular toxicity. Moreover, even by itself, nicotine is a sympathomimetic drug that elicits hemodynamic and metabolic changes that could increase the risk of acute cardiovascular events such as arrhythmias or plaque rupture and chronically increase cardiovascular disease risk by inducing dyslipidemia. The dose-response relationship between smoking and cardiovascular mortality is non-linear, suggesting that reduction in HPHC concentrations in e-cigarette aerosols may not result in proportional harm reduction and decreased HPHC exposure may be offset by increased use by individuals who believe that e-cigarettes are safer than conventional cigarettes. Thus, taken together, current evidence does not entirely support the notion that e-cigarettes are reduced harm products or effective smoking cessation devices.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Goniewicz ML, Knysak J, Gawron M, Kosmider L, Sobczak A, Kurek J, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23:133–9.
Grana RA, Ling PM. “Smoking revolution”: a content analysis of electronic cigarette retail websites. Am J Prev Med. 2014;46:395–403.
Doll R, Hill AB. Smoking and carcinoma of the lung; preliminary report. Br Med J. 1950;2:739–48.
Doll R, Hill AB. The mortality of doctors in relation to their smoking habits; a preliminary report. Br Med J. 1954;1:1451–5.
Centers for Disease C and Prevention. Current cigarette smoking prevalence among working adults--United States, 2004-2010. MMWR Morb Mortal Wkly Rep. 2011;60:1305–9.
Stewart ST, Cutler DM, Rosen AB. Forecasting the effects of obesity and smoking on U.S. life expectancy. N Engl J Med. 2009;361:2252–60.
The health consequences of smoking: a report of the surgeon general, Atlanta; 2004.
Ezzati M, Lopez AD. Estimates of global mortality attributable to smoking in 2000. Lancet. 2003;362:847–52.
Piano MR, Benowitz NL, Fitzgerald GA. Corbridge S, Heath J, Hahn E, Pechacek TF, Howard G and American Heart Association Council on Cardiovascular N. Impact of smokeless tobacco products on cardiovascular disease: implications for policy, prevention, and treatment: a policy statement from the American Heart Association. Circulation. 2010;122:1520–44.
Luoto R, Uutela A, Puska P. Occasional smoking increases total and cardiovascular mortality among men. Nicotine Tob Res. 2000;2:133–9.
Roger VL, Go AS, Lloyd-Jones DM, Adams RJ, Berry JD, Brown TM, et al. Heart disease and stroke statistics—2011 update: a report from the American Heart Association. Circulation. 2011;123:e18–e209.
Bjartveit K, Tverdal A. Health consequences of smoking 1–4 cigarettes per day. Tob Control. 2005;14:315–20.
Bhatnagar A. Cardiovascular pathophysiology of environmental pollutants. Am J Physiol Heart Circ Physiol. 2004;286:H479–85.
Bhatnagar A. Environmental cardiology: studying mechanistic links between pollution and heart disease. Circ Res. 2006;99:692–705.
Pope 3rd CA, Burnett RT, Krewski D, Jerrett M, Shi Y, Calle EE, et al. Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke: shape of the exposure-response relationship. Circulation. 2009;120:941–8. The study report a non-linear dose response relationship between smoking and cardiovacular mortality.
Pope 3rd CA, Eatough DJ, Gold DR, Pang Y, Nielsen KR, Nath P, et al. Acute exposure to environmental tobacco smoke and heart rate variability. Environ Health Perspect. 2001;109:711–6.
Schane RE, Ling PM, Glantz SA. Health effects of light and intermittent smoking: a review. Circulation. 2010;121:1518–22.
McNeill A, Brose LS, Calder R, Hitchman SC, Hajek P, McRobbie H. E-cigarettes: the need for clear communication on relative risks. Lancet. 2015;386:1237.
O’Connor R, Fenton K. E-cigarettes: spelling out the available evidence for the public. Lancet. 2015;386:1237.
Farsalinos KE, Le Houezec J. Regulation in the face of uncertainty: the evidence on electronic nicotine delivery systems (e-cigarettes). Risk Manag Healthc Policy. 2015;8:157–67.
Kosmider L, Sobczak A, Fik M, Knysak J, Zaciera M, Kurek J, et al. Carbonyl compounds in electronic cigarette vapors: effects of nicotine solvent and battery output voltage. Nicotine Tob Res. 2014;16:1319–26.
Hutzler C, Paschke M, Kruschinski S, Henkler F, Hahn J, Luch A. Chemical hazards present in liquids and vapors of electronic cigarettes. Arch Toxicol. 2014;88:1295–308.
Schweitzer KS, Chen SX, Law S, Van Demark M, Poirier C, Justice MJ, et al. Endothelial disruptive proinflammatory effects of nicotine and e-cigarette vapor exposures. Am J Physiol Lung Cell Mol Physiol. 2015;309:L175–87.
Yu G, Chen Q, Liu X, Guo C, Du H, Sun Z. Formaldehyde induces bone marrow toxicity in mice by inhibiting peroxiredoxin 2 expression. Mol Med Rep. 2014;10:1915–20.
Gulec M, Songur A, Sahin S, Ozen OA, Sarsilmaz M, Akyol O. Antioxidant enzyme activities and lipid peroxidation products in heart tissue of subacute and subchronic formaldehyde-exposed rats: a preliminary study. Toxicol Ind Health. 2006;22:117–24.
Tani T, Kogi K, Horiguchi Y. Inhibitory effects of formaldehyde inhalation on the cardiovascular and respiratory systems in unanesthetized rabbits. Jpn J Pharmacol. 1986;40:551–9.
Sandikci M, Seyrek K, Aksit H, Kose H. Inhalation of formaldehyde and xylene induces apoptotic cell death in the lung tissue. Toxicol Ind Health. 2009;25:455–61.
Zhang Y, Liu X, McHale C, Li R, Zhang L, Wu Y, et al. Bone marrow injury induced via oxidative stress in mice by inhalation exposure to formaldehyde. PLoS One. 2013;8, e74974.
Lu Z, Li CM, Qiao Y, Yan Y, Yang X. Effect of inhaled formaldehyde on learning and memory of mice. Indoor Air. 2008;18:77–83.
Rager JE, Moeller BC, Miller SK, Kracko D, Doyle-Eisele M, Swenberg JA, et al. Formaldehyde-associated changes in microRNAs: tissue and temporal specificity in the rat nose, white blood cells, and bone marrow. Toxicol Sci. 2014;138:36–46.
Sim VM, Pattle RE. Effect of possible smog irritants on human subjects. J Am Med Assoc. 1957;165:1908–13.
Schuck EA, Stephens ER, Middleton JT. Eye irritation response at low concentrations of irritants. Arch Environ Health. 1966;13:570–5.
Kerfoot EJ, Mooney TF. Formaldehyde and paraformaldehyde study in funeral homes. Am Ind Hyg Assoc J. 1975;36:533–7.
Matsuoka T, Takaki A, Ohtaki H, Shioda S. Early changes to oxidative stress levels following exposure to formaldehyde in ICR mice. J Toxicol Sci. 2010;35:721–30.
Arts JH, Muijser H, Kuper CF, Woutersen RA. Setting an indoor air exposure limit for formaldehyde: factors of concern. Regul Toxicol Pharmacol. 2008;52:189–94.
Destaillats H, Spaulding RS, Charles MJ. Ambient air measurement of acrolein and other carbonyls at the Oakland-San Francisco Bay Bridge toll plaza. Environ Sci Technol. 2002;36:2227–35.
McGwin G, Lienert J, Kennedy JI. Formaldehyde exposure and asthma in children: a systematic review. Environ Health Perspect. 2010;118:313–7.
Sakula A. Formalin asthma in hospital laboratory staff. Lancet. 1975;2:816.
Hendrick DJ, Lane DJ. Formalin asthma in hospital staff. Br Med J. 1975;1:607–8.
Tani T, Satoh S, Horiguchi Y. The vasodilator action of formaldehyde in dogs. Toxicol Appl Pharmacol. 1978;43:493–9.
Tani T, Horiguchi Y. Effects of formaldehyde on cardiac function. Jpn J Pharmacol. 1990;52:563–72.
Takeshita D, Nakajima-Takenaka C, Shimizu J, Hattori H, Nakashima T, Kikuta A, et al. Effects of formaldehyde on cardiovascular system in in situ rat hearts. Basic Clin Pharmacol Toxicol. 2009;105:271–80.
Nunn AJ, Craigen AA, Darbyshire JH, Venables KM, Newman Taylor AJ. Six year follow up of lung function in men occupationally exposed to formaldehyde. Br J Ind Med. 1990;47:747–52.
Stanek J, Symanowicz PT, Olsen JE, Gianutsos G, Morris JB. Sensory-nerve-mediated nasal vasodilatory response to inspired acetaldehyde and acetic acid vapors. Inhal Toxicol. 2001;13:807–22.
Egle Jr JL. Effects of inhaled acetaldehyde and propionaldehyde on blood pressure and heart rate. Toxicol Appl Pharmacol. 1972;23:131–5.
Wingard C, Hitchcock P, Teague RS. A survey of aldehydes with respect to their action on the blood pressure. Arch Int Pharmacodyn Ther. 1955;102:65–84.
James TN, Bear ES. Cardiac effects of some simple aliphatic aldehydes. J Pharmacol Exp Ther. 1968;163:300–8.
Myou S, Fujimura M, Nishi K, Ohka T, Matsuda T. Aerosolized acetaldehyde induces histamine-mediated bronchoconstriction in asthmatics. Am Rev Respir Dis. 1993;148:940–3.
Morris JB. Dosimetry, toxicity and carcinogenicity of inspired acetaldehyde in the rat. Mutat Res. 1997;380:113–24.
Oyama T, Isse T, Ogawa M, Muto M, Uchiyama I, Kawamoto T. Susceptibility to inhalation toxicity of acetaldehyde in Aldh2 knockout mice. Front Biosci. 2007;12:1927–34.
Appelman LM, Woutersen RA, Feron VJ. Inhalation toxicity of acetaldehyde in rats. I. Acute and subacute studies. Toxicology. 1982;23:293–307.
Perez CM, Hazari MS, Ledbetter AD, Haykal-Coates N, Carll AP, Cascio WE, et al. Acrolein inhalation alters arterial blood gases and triggers carotid body-mediated cardiovascular responses in hypertensive rats. Inhal Toxicol. 2015;27:54–63.
Conklin DJ, Barski OA, Lesgards JF, Juvan P, Rezen T, Rozman D, et al. Acrolein consumption induces systemic dyslipidemia and lipoprotein modification. Toxicol Appl Pharmacol. 2010;243:1–12.
Conklin DJ, Bhatnagar A, Cowley HR, Johnson GH, Wiechmann RJ, Sayre LM, et al. Acrolein generation stimulates hypercontraction in isolated human blood vessels. Toxicol Appl Pharmacol. 2006;217:277–88.
Awe SO, Adeagbo AS, D’Souza SE, Bhatnagar A, Conklin DJ. Acrolein induces vasodilatation of rodent mesenteric bed via an EDHF-dependent mechanism. Toxicol Appl Pharmacol. 2006;217:266–76.
Tsakadze NL, Srivastava S, Awe SO, Adeagbo AS, Bhatnagar A, D’Souza SE. Acrolein-induced vasomotor responses of rat aorta. Am J Physiol Heart Circ Physiol. 2003;285:H727–34.
Conklin DJ, Haberzettl P, Prough RA, Bhatnagar A. Glutathione-S-transferase P protects against endothelial dysfunction induced by exposure to tobacco smoke. Am J Physiol Heart Circ Physiol. 2009;296:H1586–97.
Sithu SD, Srivastava S, Siddiqui MA, Vladykovskaya E, Riggs DW, Conklin DJ, et al. Exposure to acrolein by inhalation causes platelet activation. Toxicol Appl Pharmacol. 2010;248:100–10.
Srivastava S, Sithu SD, Vladykovskaya E, Haberzettl P, Hoetker DJ, Siddiqui MA, et al. Oral exposure to acrolein exacerbates atherosclerosis in apoE-null mice. Atherosclerosis. 2011;215:301–8.
O’Toole TE, Zheng YT, Hellmann J, Conklin DJ, Barski O, Bhatnagar A. Acrolein activates matrix metalloproteinases by increasing reactive oxygen species in macrophages. Toxicol Appl Pharmacol. 2009;236:194–201.
Wang GW, Guo Y, Vondriska TM, Zhang J, Zhang S, Tsai LL, et al. Acrolein consumption exacerbates myocardial ischemic injury and blocks nitric oxide-induced PKCepsilon signaling and cardioprotection. J Mol Cell Cardiol. 2008;44:1016–22.
Ismahil MA, Hamid T, Haberzettl P, Gu Y, Chandrasekar B, Srivastava S, et al. Chronic oral exposure to the aldehyde pollutant acrolein induces dilated cardiomyopathy. Am J Physiol Heart Circ Physiol. 2011;301:H2050–60.
DeJarnett N, Conklin DJ, Riggs DW, Myers JA, O’Toole TE, Hamzeh I, et al. Acrolein exposure is associated with increased cardiovascular disease risk. J Am Heart Assoc. 2014;3.
Andre E, Campi B, Materazzi S, Trevisani M, Amadesi S, Massi D, et al. Cigarette smoke-induced neurogenic inflammation is mediated by alpha,beta-unsaturated aldehydes and the TRPA1 receptor in rodents. J Clin Invest. 2008;118:2574–82. This study reports that acrolein mediates the neurogenic effects of cigarette smoke by stimulating TRPA1 receptors.
Haussmann HJ. Use of hazard indices for a theoretical evaluation of cigarette smoke composition. Chem Res Toxicol. 2012;25:794–810.
Spiess PC, Kasahara D, Habibovic A, Hristova M, Randall MJ, Poynter ME, et al. Acrolein exposure suppresses antigen-induced pulmonary inflammation. Respir Res. 2013;14:107.
Borchers MT, Wesselkamper SC, Deshmukh H, Beckman E, Medvedovic M, Sartor M, Leikauf GD and Committee HEIHR. The role of T cells in the regulation of acrolein-induced pulmonary inflammation and epithelial-cell pathology. Res Rep Health Eff Inst. 2009:5–29.
Wheat LA, Haberzettl P, Hellmann J, Baba SP, Bertke M, Lee J, et al. Acrolein inhalation prevents vascular endothelial growth factor-induced mobilization of Flk-1+/Sca-1+ cells in mice. Arterioscler Thromb Vasc Biol. 2011;31:1598–606.
Roemer E, Anton HJ, Kindt R. Cell proliferation in the respiratory tract of the rat after acute inhalation of formaldehyde or acrolein. J Appl Toxicol. 1993;13:103–7.
Lyon JP, Jenkins Jr LJ, Jones RA, Coon RA, Siegel J. Repeated and continuous exposure of laboratory animals to acrolein. Toxicol Appl Pharmacol. 1970;17:726–32.
Schroeter JD, Kimbell JS, Gross EA, Willson GA, Dorman DC, Tan YM, et al. Application of physiological computational fluid dynamics models to predict interspecies nasal dosimetry of inhaled acrolein. Inhal Toxicol. 2008;20:227–43.
Zhang Y, Sumner W, Chen DR. In vitro particle size distributions in electronic and conventional cigarette aerosols suggest comparable deposition patterns. Nicotine Tob Res. 2013;15:501–8.
Czogala J, Goniewicz ML, Fidelus B, Zielinska-Danch W, Travers MJ, Sobczak A. Secondhand exposure to vapors from electronic cigarettes. Nicotine Tob Res. 2014;16:655–62.
Pellegrino RM, Tinghino B, Mangiaracina G, Marani A, Vitali M, Protano C, et al. Electronic cigarettes: an evaluation of exposure to chemicals and fine particulate matter (PM). Ann Ig. 2012;24:279–88.
Brook RD, Rajagopalan S, Pope 3rd CA, Brook JR, Bhatnagar A, Diez-Roux AV, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–78. The statement discusses current evidence linking exposure to particulate matter to cardiovascular disease.
Kmietowicz Z. Market for e-cigarettes includes 466 brands and 7764 unique flavours. BMJ. 2014;348:g4016.
Villanti AC, Richardson A, Vallone DM, Rath JM. Flavored tobacco product use among U.S. young adults. Am J Prev Med. 2013;44:388–91.
Kaleta D, Usidame B, Szosland-Faltyn A, Makowiec-Dabrowska T. Use of flavoured cigarettes in Poland: data from the global adult tobacco survey (2009-2010). BMC Public Health. 2014;14:127.
Gardiner P, Clark PI. Menthol cigarettes: moving toward a broader definition of harm. Nicotine Tob Res. 2010;12 Suppl 2:S85–93.
Delnevo CD, Gundersen DA, Hrywna M, Echeverria SE, Steinberg MB. Smoking-cessation prevalence among U.S. smokers of menthol versus non-menthol cigarettes. Am J Prev Med. 2011;41:357–65.
Nonnemaker J, Hersey J, Homsi G, Busey A, Allen J, Vallone D. Initiation with menthol cigarettes and youth smoking uptake. Addiction. 2013;108:171–8.
Farsalinos KE, Kistler KA, Gillman G, Voudris V. Evaluation of electronic cigarette liquids and aerosol for the presence of selected inhalation toxins. Nicotine Tob Res. 2015;17:168–74.
Tierney PA, Karpinski CD, Brown JE, Luo W, Pankow JF. Flavour chemicals in electronic cigarette fluids. Tob Control. 2015.
Grassi G, Seravalle G, Calhoun DA, Bolla GB, Giannattasio C, Marabini M, et al. Mechanisms responsible for sympathetic activation by cigarette smoking in humans. Circulation. 1994;90:248–53.
Hanna ST. Nicotine effect on cardiovascular system and ion channels. J Cardiovasc Pharmacol. 2006;47:348–58.
Benowitz NL, Gourlay SG. Cardiovascular toxicity of nicotine: implications for nicotine replacement therapy. J Am Coll Cardiol. 1997;29:1422–31. The review discusses the cardiovascular effects of nicotine.
Kaijser L, Berglund B. Effect of nicotine on coronary blood-flow in man. Clin Physiol. 1985;5:541–52.
Sjoberg N, Saint DA. A single 4 mg dose of nicotine decreases heart rate variability in healthy nonsmokers: implications for smoking cessation programs. Nicotine Tob Res. 2011;13:369–72.
Stein PK, Rottman JN, Kleiger RE. Effect of 21 mg transdermal nicotine patches and smoking cessation on heart rate variability. Am J Cardiol. 1996;77:701–5.
Harte CB. Nicotine acutely inhibits erectile tumescence by altering heart rate variability. Urology. 2014;83:1093–8.
Adamopoulos D, Argacha JF, Gujic M, Preumont N, Degaute JP, van de Borne P. Acute effects of nicotine on arterial stiffness and wave reflection in healthy young non-smokers. Clin Exp Pharmacol Physiol. 2009;36:784–9.
Neunteufl T, Heher S, Kostner K, Mitulovic G, Lehr S, Khoschsorur G, et al. Contribution of nicotine to acute endothelial dysfunction in long-term smokers. J Am Coll Cardiol. 2002;39:251–6.
Cluette-Brown J, Mulligan J, Doyle K, Hagan S, Osmolski T, Hojnacki J. Oral nicotine induces an atherogenic lipoprotein profile. Proc Soc Exp Biol Med. 1986;182:409–13.
Beere PA, Glagov S, Zarins CK. Retarding effect of lowered heart rate on coronary atherosclerosis. Science. 1984;226:180–2.
Heeschen C, Jang JJ, Weis M, Pathak A, Kaji S, Hu RS, et al. Nicotine stimulates angiogenesis and promotes tumor growth and atherosclerosis. Nat Med. 2001;7:833–9. This is the first report clearly showing the pro-angiogenic effects of nicotine.
Lau PP, Li L, Merched AJ, Zhang AL, Ko KW, Chan L. Nicotine induces proinflammatory responses in macrophages and the aorta leading to acceleration of atherosclerosis in low-density lipoprotein receptor(−/−) mice. Arterioscler Thromb Vasc Biol. 2006;26:143–9. This study shows that exposure to nicotine increase atherosclerotic lesion formation.
Vansickel AR, Weaver MF, Eissenberg T. Clinical laboratory assessment of the abuse liability of an electronic cigarette. Addiction. 2012;107:1493–500.
D’Ruiz CD, Graff DW, Yan XS. Nicotine delivery, tolerability and reduction of smoking urge in smokers following short-term use of one brand of electronic cigarettes. BMC Public Health. 2015;15:991.
Farsalinos KE, Tsiapras D, Kyrzopoulos S, Savvopoulou M, Voudris V. Acute effects of using an electronic nicotine-delivery device (electronic cigarette) on myocardial function: comparison with the effects of regular cigarettes. BMC Cardiovasc Disord. 2014;14:78.
Acknowledgments
This work was supported in part by the NIH grant HL120163 to the American Heart Association; however, the view presented does not reflect the policy of the American Heart Association or the Food and Drug Administration.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Bhatnagar declares no conflict of interest
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Additional information
This article is part of the Topical Collection on Cardiovascular Risk Health Policy
Rights and permissions
About this article
Cite this article
Bhatnagar, A. E-Cigarettes and Cardiovascular Disease Risk: Evaluation of Evidence, Policy Implications, and Recommendations. Curr Cardiovasc Risk Rep 10, 24 (2016). https://doi.org/10.1007/s12170-016-0505-6
Published:
DOI: https://doi.org/10.1007/s12170-016-0505-6