21 Days
An expert in biological warfare warns against complacency in public measures against Ebola.

“I want to be pleasant through this whole thing,” California Representative Darrell Issa said on Friday, unpleasantly, to a panel of medical experts at a congressional oversight-committee hearing. “But,” he continued, scolding from his perch, “we have the head of CDC—supposed to be the expert—and he’s made statements that simply aren’t true.”
During the tense four-hour session, the subcommittee challenged almost every element of the United States’ response to its domestic Ebola cases so far. Most pointedly, chairman Issa criticized the Centers for Disease Control and Prevention’s messages to the public.
“Doctor,” Issa said, turning slightly to address Assistant Secretary of the Department of Health and Human Services Nicole Lurie, “You can get Ebola sitting next to someone on a bus if they, in fact, throw up on you, can’t you? That’s reasonable?”
Lurie responded deliberately, after a brief pause, “The way you get Ebola is by exposure to bodily fluids, yes.”
“Okay. So. When the head of the CDC says you can’t get it from somebody on the bus next to you, that’s just not true,” Issa concluded. “When the head of the CDC says we know what we’re doing, but, in fact, healthcare professionals wearing what they thought was appropriate protective material get [Ebola], that means he’s wrong. When the head of the CDC goes on television and says sometimes less protection is better, and then has to reverse the protocol so that we no longer have nurses who have their necks exposed, that was just wrong, wasn’t it?”
“Those nurses were not protected,” Deborah Burger, a co-president of National Nurses United, responded.
Even since they were revised (“tightened”) last week, the CDC’s official guidelines for how to safely care for a person with Ebola are hazy with regard to what protective equipment must be used. It has become difficult to distinguish science from politics in the word that has gone out to the public in the wake of the domestic Ebola cases. Democratic messaging tends to be supportive of CDC handling and quelling of outbreak anxieties: If you have not had intimate contact with a person who is severely ill, you have no cause for concern. The quintessential Republican message, meanwhile, is one of mishandling and incompetence: Readily transmissible, even “airborne” Ebola virus is a legitimate concern. And, with that, obviously, comes fear. But it is not only Republican politicians who are baldly criticizing the American response to the outbreak and inconsistent public messaging.
This week I received a "monograph" for review from an unlikely, politically removed scientist. It was plainly titled "Summary of Ebola Virus Disease," and written in exhaustive scientific detail. The author was Steven Hatfill.
If the name rings a bell—I don’t want to dwell on this, but it's germane to the context of his perspective I'm sharing here—it’s because he was very publicly, very falsely accused of killing several people with anthrax in 2001.
Hatfill is rightly wary of the media that overwhelmingly convicted him in the court of public opinion, driving him to despair before his acquittal and much less-publicized redemption. But not as wary as he is of his knowledge and perspective on the Ebola outbreak going unheard. His 11,000-word textbook-like research review made several points that are contrary to the mainstream public messaging about Ebola transmission. As he wrote in an accompanying lay explanation: “The initial response to the outbreak of Ebola in the United States has been badly designed, and poorly and incompetently implemented. In their effort to minimize public concern or even panic, the leading health authorities of the United States have made far over-reaching statements and assumptions that are not fully supported by the existing scientific literature.”
For one objection, Hatfill wants it known that, while it must be emphasized that airborne droplet and particle transmission between humans has not been evident in this outbreak, aerosol droplet transmission of Ebola virus has been shown in animal studies. “It is therefore irresponsible for government health officials to emphatically state that aerosol transmission does not occur,” he writes. He also believes the argument against a national quarantine is “inexcusable in light of the size of the current West African epidemic.”
Hatfill’s concerns are backed by some compelling evidence and the clout of a long, storied career. It was actually his unique expertise in biomedical warfare—his extensive experience studying the world’s deadliest infectious agents—that led to his implication in the 2001 U.S. anthrax attacks. His training was in military special operations and tropical pathology, and after serving as an overwinter physician in Antarctica, he obtained master’s degrees in microbial genetics, medical biochemistry, and hematological pathology, including postdoctoral fellowships at Oxford University, the National Institutes of Health, and the National Research Council, in addition to over 15 years of clinical work in Africa.
In the wake of 9/11, Attorney General John Ashcroft made a rare move in publicly naming Hatfill as a “person of interest” in the investigation that desperately demanded a lead. Five people were dead and 17 sickened by anthrax sent via U.S. mail during an unprecedented crisis of confidence in domestic security. As writer David Freed recounted the story in our magazine in 2010, it was the only time an attorney general ever gave a person that designation during an active criminal investigation. The FBI trailed Hatfill everywhere he went for more than a year. Members of the media widely condemned him. Nicholas Kristof of The New York Times even implored the FBI to dig deeper on Hatfill in 2002, making outlandish accusations: “Have you examined whether [Hatfill] has connections to the biggest anthrax outbreak among humans ever recorded, the one that sickened more than 10,000 black farmers in Zimbabwe in 1978–80?”
The Kristofian character assassination of Hatfill stretched so far as to note that while Hatfill was “a true-blue American with close ties to the U.S. Defense Department, the C.I.A., and the American biodefense program”—in 2000, Hatfill was certified by the United Nations as a biological-weapons inspector for a commission in Iraq—”on the other hand, he was once caught with a girlfriend in a biohazard ‘hot suite’ at Fort Detrick, surrounded only by blushing germs.”
That was only vaguely true. In the midst of this condemnation, Hatfill became depressed, sinking into reclusive alcohol abuse. Brooding until his day in court, he took solace in studying microbiology and sculpting the lawsuits that would eventually earn him $5.8 million from the Department of Justice in addition to undisclosed settlements from media outlets. (The New York Times paid nothing, on the defense that Hatfill was a public figure and thus fairly subject to unfair accusations, but Kristof did recant artfully, six years later: “The job of the news media is supposed to be to afflict the comfortable and comfort the afflicted. Instead, I managed to afflict the afflicted.”)
One of the oddest things about the whole ordeal was that Hatfill knows relatively little about anthrax. Even though he was touted as an international expert with unique access and knowledge to the bacterium, he has always been primarily a student of deadly viruses. What he does know, at a depth that can rival any scientist’s knowledge, is Ebola.
Hatfill is currently an independent researcher with a state-of-the-art boat (in construction) on which he will conduct his own trials. He is an adjunct assistant professor at George Washington University School of Medicine, chair of the Asymmetrical Biodiversity Studies and Observation Group in Malaysia, and medical director of a London-based company with extensive contracts in the Middle East and Africa called EFP Tacmed, which operates a remote jungle-training facility to test new equipment in high-biodiversity areas. He is also a fellow of the Explorers Club and a board member of the Arizona-based nonprofit Doctors for Disaster Preparedness [Update 10/27/14: This is a controversial organization.] He has a handshake that could crack a walnut.
In the late 1990s, Hatfill finished a term at the National Institutes of Health, and began working with the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) at Fort Detrick in Maryland. USAMRIID researches vaccines, treatments, and disease pathologies, primarily to protect military service members from biological threats. (The agency boasts, on its website, “world-class expertise in the generation of biological aerosols for testing candidate vaccines and therapeutics.”) Its laboratories have specialized capabilities to research and treat the most dangerous infectious agents conceivable.
There was one other Ebola outbreak in the United States, for which the country was well prepared. It happened in 1990, when a shipment of macaque monkeys from the Philippines fell ill in the laboratories of Hazelton Research Products in Reston, Virginia. The company sent tissue samples from the animals to nearby Fort Detrick, where tests showed antibodies to Ebola virus. The macaques were evacuated to Fort Detrick by its highly trained Aeromedical Isolation Team. There they were euthanized and studied. No humans there contracted the virus, despite handling the extremely contagious tissue.
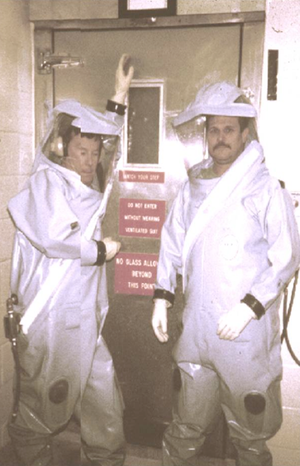
The Fort Detrick team was very experienced, and very practiced. The rapid response unit had worldwide airlift capability designed to safely evacuate and manage contagious patients under high-level containment. They knew exactly how to handle the infected macaques. In their work with primates, they had the capacity to pick up a patient overseas, put them in a mobile isolator, fly them to Maryland, and put them into the treatment facility designed for exactly this kind of outbreak. Everyone wore space suits, so it didn't matter the amount of virus that the patients were shedding into the environment. The suits were filled with air by a fan, inflated like balloons, so that if by some chance there was a tear in the suit, nothing could be sucked in to expose the person. When doctors left the isolation unit, they went through an air lock into an anteroom, where they spread their arms and were sprayed down with a glutaraldehyde-based disinfectant. The colorless liquid killed every known life form. While in that room, Hatfill recalled, those people were the cleanest things on the planet. When they came out, the suits were cut away from them and incinerated on site.

Now infected materials have to be transported by a medical-waste company. That facility at Fort Detrick was the quintessential Biosafety Level 4 (BSL-4) containment lab. But it was shuttered in 2010, a casualty of what Hatfill understands to be imprudent budgetary cuts. The World Health Organization classifies the Ebola virus in the highest-risk category of infectious pathogens, Risk Group 4, denoting that infected people should be handled with BSL-4 precautions. But since its outbreak in the United States, Ebola guidelines from the CDC have treated the virus under the much less stringent BSL-3.
For that reason Hatfill is both incredulous and seriously concerned. He believes, of course, that there is no good in panic, and that this outbreak will “burn itself out” despite yet-inappropriate handling and public messaging. But healthcare workers will contract this virus who needn’t, as more than a hundred in West Africa and two in the U.S. have. The world has to learn from this Ebola outbreak, because it will happen again on a bigger scale, and possibly with a more deadly virus, for which the United States is not properly prepared.
Pathologists at Fort Detrick concluded that the Reston outbreak was a unique strain of Ebola, which they called, aptly, Reston ebolavirus. There are currently five known species of Ebola virus: Zaire, Bundibugyo, Sudan, Taï Forest, and Reston. The ongoing west-African outbreak is of the Zaire species. Ebola is an RNA virus: seven proteins organized around a strand of nucleic acid. It exists squarely on the border of the definition of life. When the virus breaks into a human cell, the RNA directs production of a small army of seven-protein-plus-one-nucleic-acid entities.
An average of 12.7 days after exposure to Ebola virus, sudden-onset flu-like symptoms take the person. The symptoms are described as “nonspecific”—doctor-speak for saying that they could be due to tons of different things. (“I don’t know what this is.”) Those symptoms often include fever, headaches, nausea, diarrhea, sore throat, joint pain, chest pain, hiccups, shortness of breath, and difficulty swallowing.
For 4.1 percent of patients, based on mathematical modeling, the period between exposure and onset of the first symptoms is longer than 21 days. Around 13 percent of infected people in the current outbreak did not have a documented fever, according to a New England Journal of Medicine report last month. As Hatfill noted in his manuscript, researchers studying an outbreak in Uganda in late 2000 reported that "the commonest symptom … was fever, but this occurred in only 85 percent of the cases.” Another study of that outbreak found fever in only 88 percent. A study of the 1995 outbreak in the Democratic Republic of Congo found fever in 93 percent of the 84 people who died.
On the second or third days of symptoms, about half of patients develop a skin rash on their face and chest. That coincides with a generalized inflammatory response to the virus in the person’s blood. The blood pressure drops dangerously low. As the virus continues to replicate, the person’s immune system goes further into overdrive. Some of the immune cells receive false signals from the virus that tell them to kill themselves. And so they do. As in AIDS, a person’s white blood cells are destroyed, and the immune system bottoms out. Then, for some, comes the bleeding.
Because the body’s inflammatory response is in overdrive, little blood clots start forming everywhere, blocking tiny capillaries that feed vital organs. The overuse of that clotting material is doubly bad, in that the remaining blood no longer clots normally. Five to seven days after the first symptoms, people begin bleeding from their eyes, throat, and bowels. Without any supportive care, most people are dead from widespread organ failure in another two to three days.
Ebola is the prototype of an emerging infectious disease in that it is, importantly, a zoonotic virus (transmitted from animals to people). This is the route of introduction of the world’s most virulent new pathogens. During the past 30 years, to Hatfill’s knowledge, 41 new infectious organisms or strains have crossed from animal hosts into humans. The period between 2010 and 2014 alone saw the advent of the MERS Coronavirus, the Bas-Congo Rhabdovirus (which causes a hemorrhagic fever, similar to Ebola), ongoing Monkeypox outbreaks, and a rash of Ebola in the Democratic Republic of Congo, in addition to the ongoing West African Ebola outbreak.
The risk for human infection by these viruses depends, initially, on human-animal interactions. Bats are a prime example of a reservoir for RNA viruses that cross between species and infect people. Those the sub-order that include the now-notorious fruit bats have been implicated in RNA-viral outbreaks among the most lethal infectious diseases: Ebola, Marburg, Hendra, Hipah, SARS, MERS, and the Australian lyssaviruses. Those interactions are driven by the expanding human population (which has doubled worldwide in the past three decades). They are also driven by animal-habitat fragmentation, losses in biodiversity, and war.
Many of the deadly emerging RNA viruses arise, as Hatfill makes clear in his work, from biodiversity hotspots—regions that house at least 1,500 species of vascular plants and have lost at least 70 percent of their vegetation. These biodiversity hotspots are home to more than half of the world's plant and non-fish animal species, as well as more than a billion of the world’s poorest people. The regions also involve more than 90 percent of recent armed conflict. Refugees hunt for meat and build remote encampments, increasing pressure on local resources and interfering with wildlife, drawing people into the line of fire between the viruses and their animal reservoirs. And so it is there that Hatfill believes efforts to manage inevitable future outbreaks must focus.
What follows is a condensed transcript of our conversation last week in Washington, D.C. It’s still long, but I decided to err on the side of including information. His message is, again, not intended to panic, but to provoke nuanced evaluation of the scientific evidence around Ebola transmission, and whether or not we are truly prepared for the inevitable viral outbreaks of the future.
Steven Hatfill: For the last at least 30 years, scientists have been very, very worried about emerging infectious diseases. And we've been seeing outbreaks of things we'd never seen before at an alarming frequency over the last few years. Right now we're looking at about five agents, several of which we've never seen before. The Bas-Congo virus is a rabies-type virus transmitted by bats through their droppings, we assume. It's a hemorrhagic fever; it kills you in two to three days from the start of symptoms. This is Ebola on wheels. [Ed: There have been only three known cases.]
There is also the MERS virus outbreak in the Middle East. And Coronavirus, we'd never seen before, came in from the camels imported into the UAE and Saudi Arabia. The outbreaks of monkeypox in Kasai Oriental Province, that's ongoing. An Ebola outbreak right now in Democratic Republic of the Congo. We've got a Chikungunya epidemic in Puerto Rico, outbreaks in Florida, a secondary case that indicates the mosquitoes are transmitting it. And dengue. It's in the albopictus mosquito, the Asian tigers, and we assume it's going to move north in Florida.
James Hamblin : And population density is the driving factor of these new infectious-disease outbreaks?
Hatfill: For dengue and chikungunya, yeah. People that have been trapping bats and other animals in these high biodiversity areas are finding viral sequences, and we don't know what they're from. This is not in the GenBank database. So there are things lurking out there we don't have a clue about. How do you get a rabies virus that causes hemorrhagic fever? Well, going back through the literature, there's a fish virus that can cause hemorrhagic septicemia. The frequency that these things are happening is very disturbing. Just remember, our population's doubled in 27 years. So you encroach on animal habitats, or you fragment those animal habitats, you disrupt the ecology, the normal food sources.
At the moment, it's the fruit bats. And their range extends way past Africa, the ones that are transmitting this. We found Ebola Zaire antibodies in bats in Bangladesh, and as far over as Borneo, although that paper needs some reassessment. [Ed: There is evidence that filoviruses (Ebola among them) may be harbored across a larger geographic range than some previously assumed. Contested evidence of Ebola Zaire has been reported in orangutans in Borneo.] So that's a huge swath of land down into northern Australia, India, and over. So the more these habitats become fragmented, and the bats move closer to humans—the fruit bats, especially. You cut down their forest, you build orchards, where are they going to go? To the orchards. And these bats are carrying everything from the Hendra virus in Australia, that unusual outbreak in the mid-90s, to the Nipah virus in Malaysia. And we're going to put 4,000 troops in the middle of this habitat. Are you going to tell the bats not to poop on the soldiers?
Hamblin: I could tell them, but I don't think they'd listen.
Hatfill: No, I don't either. So it's a problem.
Hamblin: I wanted to ask about your work at Fort Detrick. Excellent conditions for research, with lots of years that we had there to develop a treatment or vaccine, but we don't have one.
Hatfill: We went down a wrong path. ... But again, funding is intermittent. And with the sequestration, we're not even training Navy SEALS in combat-casualty care anymore. You had this whole unit that was ready for some type of emerging disease, whether it was Ebola or whatever, completely unknown. And they practiced. The Walter Reed people would come up and put on the space suit. I know because I was a patient once, a simulated patient. And they fly you in the isolator. And the isolator hooks up to the outside of the building and seals. And then they drag you inside the BSL-4 treatment area. So, I mean, you couldn’t do better than that. It's an Andromeda strain. And then it's gone.
Hamblin: Totally gone?
Hatfill: Yeah. You could change the airflow around Fort Detrick and bring it back, but you still wouldn’t immediately have the experienced people who have rehearsed protocol for years. Intubation [placing a breathing tube down a dying patient’s throat] is difficult enough. You ever tried to do it in a space suit?
Hamblin: No.
Hatfill: So you practice these things. And develop a sense of calm. You don't take a nurse that's just come out of ICU training and then say, "Yeah, you go in there." You'd be crapping yourself. You need very experienced people that are used to it, and you need appropriate guidelines. We've taken a BSL-4 disease, and we're treating it in BSL-3 conditions. Because they did it in Africa. Well, outside is a much different story than inside. Outside, these viruses, if they do get airborne, they don't last long. They're subjected to oxidation by the oxygen in the air. Osmotic stress from the ambient humidity in the air and ultraviolet light. Plus they're open-air hospitals, so [the viruses] blow away. That's different than in an enclosed room.
So when I heard Anthony Fauci [director of the National Institute of Allergy and Infectious Diseases] say, yeah, one glove is sufficient, I just lost my mind.
Hamblin: There were claims, I'm not sure the origin of them, after the first Dallas nurse contracted Ebola, that it was maybe because she wore too much protective gear. I didn’t understand what that meant.
Hatfill: That's just complete nonsense. Look how they dress in Africa, and look at the first CDC guidelines. There's no comparison. You wear hoods. You wear masks and hoods over them. You wear goggles. You're getting sprayed when you come out and you're walking through a little kiddie pool filled with bleach. So the outside of your suit is being decontaminated before you try to take it off.
Hamblin: So what led to us treating it with such relative casualness? The CDC not having experience with Ebola in the U.S.?
Hatfill: [Thomas Frieden, CDC director] has become a political animal, in my opinion. And when you're dealing with this type of agent with no cure, no real vaccine, you must always err on the side of caution. They ignored a lot of published data. We've known for years now that the skin is a site of viral replication. The Langerhans cells, the antigen-presenting cells in the skin, are major targets for Ebola. The strains we know of.
What that means is, you're shedding virus from the skin to the point where Bob Swanepoel [a professor of medical virology at University of Pretoria] and some people actually found you could come up, take a swab, just a cotton swab off the skin, and diagnose [Ebola] with a non-PCR method, something like immunohistochemistry, and get a positive result from a live virus.
Hamblin: So you’re saying there is at least some evidence that a person could brush up against someone and contract Ebola virus?
Hatfill: People have touched the bed of a patient and caught this, after the patient died and was removed. They brushed up against the bed and caught it. [Ed: Such a bed would need to be grossly contaminated, according to the vast majority of evidence.]
Hamblin: You write that as few as 10 Ebola virus particles could cause human infection, though that number needs more research. Everyone is sticking very hard to the message that unless you've come in contact with the bodily fluid—
Hatfill: Here's the problem. You don't want to panic everyone. And [the CDC leaders] were at a loss that their [preventive] procedures didn't work and this happened and the leadership were shocked. You don't want to panic people, but people aren't stupid. You see people wearing semi-space suits taking these patients into hospitals, and everyone's telling you there's no aerosol transmission.
In the classical outbreaks of Ebola, there has been no evidence of aerosol transmission. That nurse and lab technician who handled the blood from the first guy, Duncan, I'm sure his blood went to the lab and he had a full blood count at his first admission. Well, Coulter counters [machines used to perform blood tests] are notorious for making little aerosols. And the fact that nobody in the laboratory came down with it is, yay. So we haven't seen aerosol transmission, classically, in all these smaller outbreaks for the last 30 years. And it's assumed that it wasn't transmitted aerosol. But that doesn't mean that it can't be under conditions. And we really don't know the amount of viral shedding. C.J. Peters [distinguished chair in tropical and emerging virology at the University of Texas Medical Branch] and other people have found live virus in saliva, tears, and nasal secretions.
So to say it's not aerosol transmitted is irresponsible. People aren't stupid. Look at Ebola Reston. When that broke out, a lot of people were thinking this was aerosol-transmitted because several people seroconverted [showed evidence of Ebola exposure in their blood]. But not one of them got sick. We found in Fort Detrick the Reston strain doesn't attack the lining of your blood vessels, and your own immune system just hoofs it.
Hamblin: But it was some evidence of a possible aerosolized mode of transmission? [Ed: More on the specifics of droplet transmission here.]
Hatfill: It was suggestive. Late experiments took some Landrace strain pigs—the cute little Green Acres ones—and infected them nasally. They put the infected pigs in with some uninfected pigs, and they all contracted it. In pigs, it gives them a very severe respiratory disease.
Then they took Ebola Zaire, and they mixed nasal secretions of uninfected pigs and primates together, and the primates got it. Now, none of the primates passed it between them. So we're talking about viral shedding, and the question is, how much virus is being secreted from what sites, what fluids? There are a lot of unknowns. Most particularly, when does viral shedding start?
Hamblin: And what we're hearing most commonly is that it's around when a person develops a fever.
Hatfill: Well, 12.5 percent of patients don't run a fever. In that New England Journal of Medicine study, where they just looked at several thousand of these cases in West Africa, the lead author of the paper is adamant. He says, I sat there, I monitored this patient's temperature myself until they died and they never ran a fever. Well, generating a fever is a fairly complex mechanism in your body. Neutrophils and cytokines are involved. One of the things a virus does is it inhibits neutrophil activation. Ebola's outer glycoprotein can secrete a truncated version of it. You've seen the planes come over and shoot out the flares so the missile can't get them. That's what Ebola's doing. It's shooting out these little truncated bits of glycoprotein as flares. It's masking itself. Indirectly, its inhibiting neutrophil activation, and what they release tell us to run a fever.
Hamblin: So the neutrophils attack that flare.
Hatfill: They're getting confused by it.
Hamblin: And the immune system says, it's not a big deal, everything's okay.
Hatfill: And they're not releasing pyrogens. This is our best guess. We need to get it in the lab and have a better look at it. And it's not just the West African outbreak. The other outbreaks have reported the same thing fairly consistently. So to use this as a screening measure rather than quarantine measures becomes problematic.
Hamblin: Is there any other better screening measure that could be considered?
Hatfill: We have rapid PCR tests. Texas had them, but they're not allowed to use them because the FDA never certified it. We have a classified set of Department of Defense primers for PCR that work great.
Hamblin: So any hospital cannot handle patients with Ebola. What do we do with the people who have it? What should be done with the future cases in the U.S.?
Hatfill: The CDC put out inadequate guidelines, and now they have to admit it. So everybody's backtracking. The generation before me classified Ebola as BSL-4. That's safe. We've been working with it for years.
Hamblin: Don’t we have facilities that can handle BSL-4 infectious disease?
Hatfill: We only have a handful, and they're not geared up for patients. Now, USAMRIID could change it back over quickly, but the most they could handle would be one or two patients. But instead of [investing in] that, we went out and built all new research centers. We've wasted $120 billion over the last 20 years. Nothing to show for it. We can't even handle one patient with Ebola.
Chikungunya is Swahili for “walks bent over.” It attacks the synovial membranes in your joints. It's agonizing. In fact, you're afraid you won't die. But most people get through it. It was, a hundred years ago, a fairly benign disease. There was a lot of travel between India and Durban in South Africa. Commerce, personnel, people, immigrants, back and forth. And the population density ramped up. It’s an RNA virus—you won't find an RNA virus that has more than about 10 genes or so, because any more than that it's made so many mistakes as it's replicated its genome, it's nonfunctional. So it doesn't get propagated. Some time over the last 100 years, one of these strains had a single mutation that enabled it to replicate to a higher titer inside the mosquito, and now that's the dominant form, which means these patients are getting a higher dose of virus. As with any infectious disease agent, the bigger dose you're exposed to, the quicker and more severe are going to be your symptoms.
Hamblin: You write about the role of conflict and war in viral outbreaks.
Hatfill: Eighty percent of the conflicts fought since 1953 have been in stressed high-biodiversity areas. This is asking for trouble. … You put your troops in there and wonder why they get Korean hemorrhagic fever in Korea. I don't know where those fruit bats have gone. They're migrating at the moment. This is why there are these periodic outbreaks here and there.
Hamblin: The idea of a travel ban has been so controversial.
Hatfill: Not to other countries.
Hamblin: To the U.S. it has.
Hatfill: When the SARS epidemic happened, Singapore came very close to being wiped out. People don't realize this. And over there, if you chew gum or spit on the street, they cane you. Singapore had this under control overnight, and all their contact tracings were confined to their house, to the point where they would phone you every hour and you'd better answer the phone or the cops came by to arrest you. And they stopped it. You saw in the U.S. the journalist went out for pizza, this nurse went on a plane. Are you out of your mind? Though in a way this is good, because it shows aerosol and skin shedding in early infection is not occurring.
The cops went in to check Duncan's apartment without any personal protective equipment. His family members didn't come down with it. Again, this is like, whew. Kinda dodged a bullet there.
Hamblin: When you talk about aerosol potential, you mean in respiratory droplets?
Hatfill: That's what is normally referred to. Here's the thing. The antigen-presenting cells in the body are major targets for Ebola, and we find these everywhere. Our throat, the Waldeyer’s ring, is full of antigen-presenting cells. Its job is to check everything coming into my airway and my mouth, show it to its buddies, and determine, "Should I be alarmed?" "No, no." Or, "Oh, no, we're going to make an immune response." Bronchial-associated lymphoid tissue, skin-associated lymphoid tissue, gut-associated lymphoid tissue: All these portals to the outside world are protected by these sentries. The virus likes to attack the sentries and replicate in them to [a] high concentration.
So physiologically, biomedically, yes, it looks like it's possible. Epidemiologically when we look at it, we don't appear to see it. But don't get up and say, "Cannot occur." That's nonsense. And people aren't stupid. They see everyone running around in Tyvex and positive-pressure respirators, and they're going, what they heck is going on here? Don't dumb it down. Tell people: The animal data shows this can happen, [and] we're looking for it. We haven't seen any indications at this time.
The other thing Singapore did was put in the thermal scanners [at airports] immediately, like the next day. They're commercially available. It's so unobtrusive you can't even tell, but, oh, yeah, there it is over there. And you can see your thermal image. We waited to the last minute to do it. Why? You have you err on the side of caution, especially when you have 317 million people in close proximity and a very good infrastructure. You can be from here to there in 6 hours. You can be from the Congo to JFK in 24.
Hamblin: Travel-ban opposition is largely based on the claim that it would impede our ability to help stem the epidemic in West Africa.
Hatfill: You know, I went for a Department of Defense interview years ago. They wanted a scientist down at the Pentagon that could invent stuff that would support presidential policy. ... They just wanted a spokesperson that could kind of come up with a plausible explanation to explain a higher-up directive. And I think this is the same thing.
Hamblin: I'm wondering what is driving—
Hatfill: There are no cases in Kenya.
Hamblin: And they have a travel ban?
Hatfill: Yes.
Sanjay Gupta, who is a neurosurgeon, did probably the best demonstration I've seen on why the CDC protocol failed. He dressed up in the recommended protective equipment and they put chocolate syrup on his hands. As an experienced neurosurgeon, how many times he's donned and doffed this gear? He took off his gear, and, yep, there were chocolate splashes all over his skin. There's a reason we use front-zipping Tyvek suits and not gowns. If an experienced neurosurgeon can't do it, what do you think a poor gal just out of ICU training is going to do?
The nurse that got infected knows she's in there with an Ebola patient, and God bless her for volunteering to do this. It's a very, very brave thing to do. But it's not just issuing a guideline. You have to practice implementing it. And the whole hospital has to practice. You can't come up with it at the last minute.
Hamblin: Do you think this outbreak will—
Hatfill: It'll burn itself out. Nigeria's already got control over theirs. Why? They follow the rules.
Hamblin: Is this a a wake-up call for the U.S.?
Hatfill: If it isn't, then we're doomed. Dr. Hamblin, there are worse things out there. Again, we're finding viral sequences, and we don't know what these are from. There are other things out there.
Hamblin: How do we get the government to invest in emerging infectious disease preparedness?
Hatfill: We spent 120 billion on this, on emerging disease and bioterrorism, what have we got to show for it? Machines that the FDA hasn't licensed for rapid diagnosis.
Hamblin: I don't understand where the money you mention is going.
Hatfill: It disappeared. It just disappeared.
Hamblin: I don't know what that means.
Hatfill: We have nothing to show for it. … Mother Nature is not happy with us at the moment.
Hamblin: So you think this is a tip-of-the-iceberg situation, this outbreak?
Hatfill: Here's a very good example. In 1993, 1994 somewhere I think in that timeframe, we almost lost every lion in the Serengeti. The Distemper virus jumped from the wild African dogs into the great cats and it slaughtered them. They had no immunity. And they had to go in and vaccinate wild lions.
Hamblin: They did that with darts?
Hatfill: I forget how they did it.
Hamblin: They could tranquilize them.
Hatfill: I heard rumors of infected meat. I don't know how that would work. But 80, 90 percent of the population crashed. Mother Nature tends to do that. We're not there yet. But when's our next doubling time for population?
Hamblin: It's not long. I know the over-65 population in the U.S. is doubling in the next 25 years.
Hatfill: With poor immune systems because they're older, susceptible to all sorts of stuff. And now China's moving everybody into high-density urban areas. They built these huge cities, million person cities, and there's nobody in there. And they're going to relocate their rural population. Why? Because it stimulates consumer spending and provides jobs. This is their grand plan. Well this is where all the flu viruses mix and come from. God knows what that will generate. This is a serious problem. It's not something that can be ignored any longer.
Hamblin: You said not many hospitals can handle a case. I saw the number six thrown around. Do you think it's that low?
Hatfill: Depends on how much they practice. And if it's not mandated, hospital administrators aren't going to do it. They're stressed as it is.
Hamblin: It's a tough investment to justify until a threat is imminent.
Hatfill: Exactly. You want me to do what? Practice what? You know, that's going to cost the hospital. So I mean, this is for-profit medicine in this country, unfortunately.
Hamblin: Speaking of the for-profit: Pharmaceutical companies, they're not going to factor into development of vaccines and treatments of emerging infections diseases.
Hatfill: Well no, because the majority of [Ebola] patients don't have any money. These are businesses. Fair on them, it's a business, right? ... Do we have enough Tyvek suits? This was a thing that was brought up yesterday evening during a meeting. Dupont can make these things, we can crank them out and we can double our capacity, but if the epidemic ends we've just outlaid millions to ramp up capacity. Who's going to pay us? Because we're not going to do it on our own, we're a business.
… So there are positive signs here, and it's not the sky is falling, but dammit, animal data is pretty convincing that this is a possibility. Don't tell people it's not. Be honest with them. "Yes, we've had some animal studies, it's shown this, but I have to reaffirm we have not seen this to date."
Though Hatfill preferred that I not mention geographic specifics, he is consulting to African countries on Ebola containment and prevention. Shortly after our conversation, he left the U.S. to answer the calls for policy help from long-standing contacts established over his 15-plus years of work in Africa.
His advice to the CDC, though no one has asked him for it, centers on the fact that as new antiviral treatments are developed, the need for rapid medical response units will become paramount. These treatments have to be administered quickly, but they could stem outbreaks before they become significant. Medical response units would need to be able to enter remote areas for on-site diagnosis and administration of antiviral medication. They would need isolation transportation and BSL-4 treatment facilities in the United States. Because outbreaks like this one will happen again, and they are best addressed by focusing containment and treatment efforts at the source of the outbreak.
With the right military crew properly equipped, he said, smiling at the thought, "They'd love doing it. I guarantee it. Hell, I'd like to be on one. It depends if we're going to take this as a wake-up call or not."
A response to this post, with further clarification of some studies mentioned, is here.