Scientists have edged closer to a therapy for muscular dystrophy by turning skin cells from a patient into healthy muscle cells.
Researchers hope injections of the newly made cells could boost the performance of failing muscles in patients and so alleviate some of the worst symptoms of the condition.
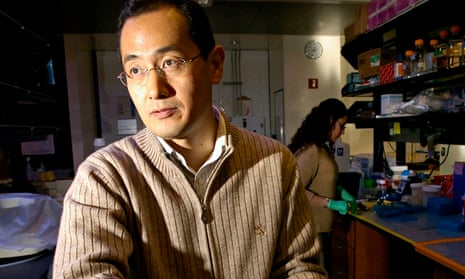
The work, led by Shinya Yamanaka, who won the Nobel prize in 2012 for discovering that adult cells can be reprogrammed into a younger state, shows that genetic mutations that cause Duchenne muscular dystrophy can be safely corrected using a powerful new procedure called genome editing.
Duchenne muscular dystrophy is a degenerative disease that affects one in 3,500 boys and normally proves fatal by early adulthood. It is caused by mutations in a gene that makes a protein called dystrophin. Without the protein, muscle fibres become damaged and waste away.
Yamanaka’s group at Kyoto University took skin cells from a patient with Duchenne muscular dystrophy and converted them into immature cells, known as induced pluripotent stem (iPS) cells. These cells can be nudged into forming a range of other cell types.
The scientists took batches of iPS cells made from the patient’s skin and tested three different genome-editing procedures to correct the faulty dystrophin gene. They found two approaches, Talen and Crispr, could repair the damaged gene. Both use enzymes to remove faulty genetic material before replacing it with corrected DNA.
By creating healthy muscle cells from the patient’s skin cells, the scientists avoid any risk of the cells being rejected by the patient’s immune system. Unlike traditional gene therapy, the faulty gene is corrected in cells outside the body so they can be screened to make sure the genetic modification is safe before being returned to the body.
Even though scientists have no hope of correcting all of the muscle cells in a patient’s body, injections of healthy cells could provide enough dystrophin to boost their existing muscle tissue. Many patients have trouble breathing, chewing and swallowing, so strengthening those muscles could have a dramatic impact on quality of life.
“Genetically corrected muscle cells or muscle progenitor cells should be able to fuse with muscle fibres,” said Akitsu Hotta, a senior author on the study, published in Stem Cell Reports. “Muscle fibres consist of hundreds or thousands of muscle cells, and even a few genetically corrected cells will be able to provide functional dystrophin protein for the entire muscle fibre. It would be very challenging to correct all the muscle fibres in the whole body, so the initial attempt should be focused on local muscles.”
Chris Mason, professor of regenerative medicine at UCL, said: “It’s a lovely approach. If these cells integrate into muscle in animals I’d expect it to work in humans because skeletal muscle is skeletal muscle. You don’t need to correct everything. If you can improve muscle strength by a small amount, you can help people in normal daily activised.”
Marita Pohlschmidt, director of research at the Muscular Dystrophy Campaign, said: “A number of promising potential treatments for Duchenne muscular dystrophy are currently in clinical trial. However, most of these will only result in a partially functioning dystrophin protein being produced. Using DNA enzymes to repair genetic mutations is a fast-moving research field.
“This technique has the potential to repair the genetic defect in a way that allows a fully functional protein to be made. It has the potential to develop into a treatment with a long-lasting effect, meaning children and young people may not need to be given regular treatment. However, further work and safety-testing is needed before this technology can be taken into clinical trials.”




Comments (…)
Sign in or create your Guardian account to join the discussion